ED Facility Coding Guidelines provide standardized protocols for coding emergency department services, ensuring accurate billing and compliance․ Developed by organizations like ACEP, these guidelines help facilities assign appropriate levels of care based on patient needs and resource utilization․
1․1 What are ED Facility Coding Guidelines?
ED Facility Coding Guidelines are standardized protocols designed to ensure accurate and consistent coding of emergency department services․ These guidelines outline the rules and principles for assigning appropriate levels of care, reflecting the intensity of resources and services provided․ They differ from professional coding, which focuses on physician services, by emphasizing facility-specific factors such as medical decision-making (MDM), time spent, and resource utilization․ The guidelines are regularly updated, with significant changes in 2023 aligning ED codes (99281-99285) with office and outpatient E/M coding standards․ Developed by organizations like ACEP, these guidelines help facilities comply with regulatory requirements and optimize reimbursement․ They also provide a framework for distinguishing between varying levels of care, ensuring that coding aligns with patient acuity and service complexity․ By standardizing coding practices, ED Facility Coding Guidelines promote transparency, accuracy, and fairness in billing for emergency services․
1․2 Importance of ED Coding Guidelines
The importance of ED Coding Guidelines lies in their role in ensuring accurate billing, compliance, and optimal reimbursement for emergency department services․ By standardizing coding practices, these guidelines help facilities avoid errors, reduce audit risks, and maintain financial integrity․ They also ensure that the level of care provided aligns with patient needs, reflecting the intensity of resources and services utilized․ This alignment is crucial for fair reimbursement and resource allocation․ Additionally, ED Coding Guidelines promote transparency and consistency across healthcare facilities, enabling benchmarking and performance improvement․ They also support compliance with regulatory requirements and payer policies, reducing administrative burdens․ By providing clear frameworks for coding based on medical decision-making (MDM) and time, these guidelines streamline documentation processes and enhance efficiency․ Overall, ED Coding Guidelines are essential for maintaining operational integrity, ensuring patient care is appropriately reflected in billing, and supporting the financial sustainability of emergency departments․

Key Principles of ED Facility Coding
The key principles of ED facility coding emphasize accuracy, compliance, and consistency․ They focus on standardizing coding practices to reflect the level of care provided, ensuring proper documentation and billing․ These principles guide facilities in assigning appropriate codes for emergency services, ensuring alignment with regulatory requirements and payer policies․ They also highlight the importance of distinguishing facility coding from professional coding, ensuring each aspect is appropriately documented․ By adhering to these principles, facilities can optimize reimbursement, reduce errors, and maintain operational efficiency․ These guidelines are foundational for ensuring that emergency department coding is both ethical and sustainable․
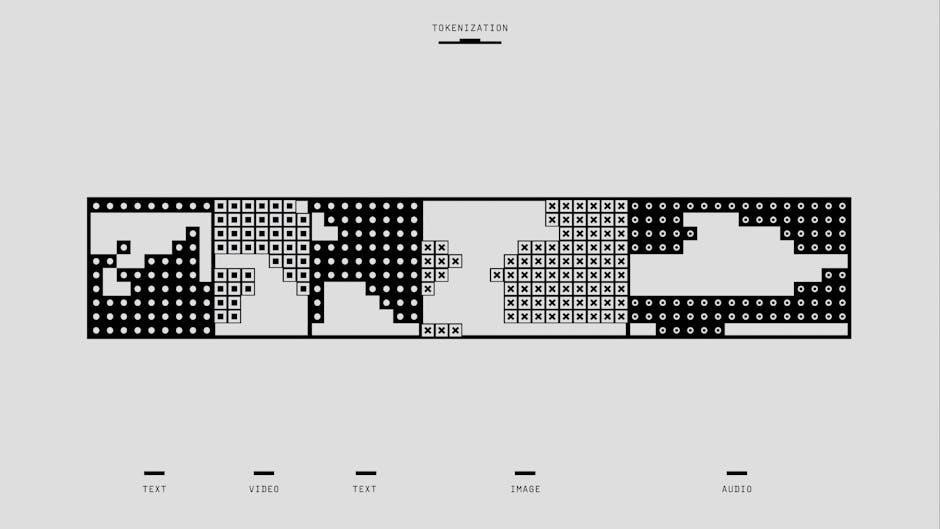
2․1 Overview of Facility vs․ Professional Coding
Facility coding and professional coding are two distinct aspects of emergency department (ED) coding, each serving a specific purpose․ Facility coding focuses on the services and resources provided by the ED itself, such as equipment, staff, and facility-related expenses․ It typically involves assigning codes for facility-based services like emergency room visits, observation care, and other hospital-based procedures․ Professional coding, on the other hand, pertains to the services provided by healthcare professionals, including physicians, nurse practitioners, and other licensed clinicians․ This involves coding for evaluations, treatments, and medical decision-making performed by these professionals․ Understanding the distinction between facility and professional coding is crucial for accurate billing and compliance․ Facility coding often uses HCPCS or CPT codes to represent facility services, while professional coding relies on CPT and ICD-10 codes to document clinical services․ Both are essential for capturing the full scope of care provided in the ED setting․

2․2 CPT Codes for ED Services

Current Procedural Terminology (CPT) codes play a critical role in coding emergency department (ED) services․ These codes are used to report medical, surgical, and diagnostic services provided in the ED setting․ CPT codes for ED services are specifically designed to capture the unique nature of emergency care, which often involves unscheduled visits and varying levels of complexity․ Common CPT codes used in ED coding include 99281-99288, which represent different levels of emergency department visits based on patient acuity and resource utilization․ These codes take into account factors such as medical decision-making (MDM), patient history, physical exams, and the time spent by healthcare providers․ Accurate assignment of these codes ensures proper reimbursement and reflects the intensity of care provided․ Proper documentation of patient encounters is essential to support the selection of appropriate CPT codes․ Understanding the guidelines for assigning these codes is vital for compliance and accurate billing in the ED setting․
2․3 Role of Medical Decision Making (MDM) and Time in Coding
Medical Decision Making (MDM) and time are pivotal elements in coding emergency department (ED) services․ MDM refers to the complexity of diagnoses, treatments, and management decisions made during patient care․ It involves assessing the number of diagnoses, the complexity of the patient’s condition, and the risk of complications․ Time, on the other hand, is measured by the duration of face-to-face interaction between the provider and the patient, including time spent on evaluation, counseling, and coordination of care․ Both MDM and time are used to determine the appropriate level of care for coding purposes․ For instance, time-based coding is applied when the provider spends a significant amount of time with the patient, while MDM-based coding focuses on the complexity of medical decisions․ Accurate documentation of these elements ensures compliance with coding guidelines and supports proper reimbursement․ Understanding how to integrate MDM and time into coding is essential for accurate and efficient ED facility coding․

Recent Updates to ED Coding Guidelines
The 2023 updates to ED coding guidelines focus on clarifying evaluation and management (E/M) codes, emphasizing accurate documentation and reimbursement for emergency services․ These changes aim to enhance coding precision and compliance․
3․1 2023 Changes to E/M Coding
The 2023 updates to E/M coding introduced significant changes to how emergency department (ED) services are coded, particularly for facility coding․ These updates aimed to simplify the coding process while ensuring accurate reimbursement for ED services․ One key change was the refinement of evaluation and management (E/M) codes to better align with the complexity of care provided in emergency settings․ The revised guidelines emphasized the importance of documenting medical decision-making (MDM) and patient acuity to determine the appropriate E/M level․
Additionally, the updates addressed ambiguities in prior coding guidelines, providing clearer definitions for levels of care and reducing redundancy in documentation requirements․ These changes also introduced new codes to reflect the unique demands of emergency care, ensuring that coders can accurately capture the intensity of services provided․ The 2023 updates underscored the need for precise documentation to support coding decisions, ensuring compliance and appropriate reimbursement for ED facilities․
Overall, the 2023 E/M coding changes streamline the coding process, reduce administrative burdens, and improve the accuracy of facility coding in emergency settings․
3․2 Impact of Updates on Facility Coding
The 2023 updates to E/M coding have significantly influenced facility coding practices in emergency departments․ These changes have prompted facilities to adapt their coding processes to align with the new guidelines, ensuring accurate reimbursement and compliance․ One notable impact is the increased emphasis on precise documentation of patient acuity and medical decision-making (MDM), which are now critical for determining the appropriate level of care․
Facilities have also experienced a shift in how they approach coding education and training․ Coding staff must now undergo updated training to understand the refined E/M codes and their application in emergency settings․ This has led to improved coding accuracy and reduced errors, ultimately enhancing operational efficiency․
Moreover, the updates have streamlined the coding process, reducing administrative burdens and allowing facilities to focus more on patient care․ However, the transition has required significant effort and resources to ensure compliance with the new guidelines․
Overall, the impact of the 2023 E/M coding updates on facility coding has been profound, driving improvements in documentation, accuracy, and efficiency while necessitating ongoing adaptation and training within ED facilities․
3․3 Transitioning to New Guidelines
Next, facilities must provide comprehensive training to coding staff and clinicians․ This training should focus on the practical application of the new guidelines, emphasizing areas such as updated E/M codes, MDM criteria, and time-based coding rules․ Regular updates and feedback sessions can help address challenges and ensure consistent implementation․
Additionally, facilities should update their coding tools and software to reflect the new guidelines․ This may include revising coding templates, implementing new coding logic, and ensuring that electronic health records (EHRs) are aligned with the updated requirements․
Finally, facilities should monitor coding accuracy and reimbursement impacts during the transition period․ By maintaining open communication with coding experts and staying informed about regulatory updates, facilities can successfully adapt to the new guidelines and optimize their coding processes․

ACEP Facility Coding Model

The ACEP Facility Coding Model provides standardized guidance for coding emergency department services, ensuring accurate reimbursement and compliance with regulations․ It complements professional coding by focusing on facility-specific coding requirements and documentation standards․
The ACEP (American College of Emergency Physicians) Facility Coding Guidelines are a comprehensive framework designed to standardize the coding practices for emergency department (ED) facilities․ These guidelines aim to ensure accurate and consistent coding, which is critical for proper reimbursement and compliance with regulatory requirements․ Developed specifically for ED settings, the ACEP guidelines address the unique challenges faced by facilities in coding emergency care services․ They emphasize the importance of precise documentation and the use of appropriate codes to reflect the complexity and intensity of ED encounters․ By aligning with industry standards and updates, the ACEP guidelines help facilities navigate the complexities of coding, ensuring that services are accurately represented and reimbursed․ These guidelines are regularly updated to reflect changes in coding regulations and clinical practices, making them a reliable resource for ED facilities․
4․2 Three Key Components of the ACEP Model
The ACEP Facility Coding Model is structured around three key components that guide accurate and consistent coding for emergency department services․ The first component focuses on the clinical presentation and acuity of the patient, emphasizing the importance of documenting the severity of the condition and the urgency of care required․ The second component revolves around the time and effort invested in patient evaluation and management, including the duration of physician-patient interaction and the complexity of services provided․ The third component highlights the resources and interventions utilized during the encounter, such as diagnostic tests, treatments, and consultations․ These three components work together to ensure that coding reflects the full scope of care delivered in the ED, enabling facilities to assign appropriate levels of service and secure accurate reimbursement․ By integrating these elements, the ACEP model provides a balanced and practical approach to facility coding․
Assigning Facility Levels of Care
Assigning facility levels of care involves evaluating patient acuity and services provided․ Factors such as patient condition, resource use, and documentation guide level determination, ensuring accurate coding and reimbursement under ED guidelines․
5․1 MDM-Based Level Assignment
Medical Decision Making (MDM) is central to assigning facility levels of care in emergency departments․ It evaluates the complexity of patient encounters, focusing on three key components: diagnoses/management options, data complexity, and risk of complications․ Higher levels of care are assigned when MDM involves multiple diagnoses, extensive data review, or high-risk scenarios․ Accurate documentation of these elements ensures proper coding and reimbursement, reflecting the patient’s acuity and the resources utilized․ This approach aligns with standardized guidelines, providing a consistent framework for level assignment based on clinical judgment and patient needs․
5․2 Time-Based Level Assignment
Time-based level assignment is another critical method for determining facility levels of care in emergency departments․ This approach focuses on the total time a patient spends in the ED, from registration to discharge, including all evaluation, treatment, and observation periods․ The duration of the visit helps estimate the resources used and the complexity of care provided․ For example, longer visits often correlate with higher levels of care, as they may involve more extensive evaluations, multiple interventions, or prolonged monitoring․ Time-based assignment is particularly useful in cases where the medical decision-making (MDM) component is less pronounced but the patient requires extended observation or care․ Facilities must document the total time accurately to support the level of care assigned, ensuring compliance with coding guidelines and proper reimbursement․ This method complements MDM-based assignment by providing an objective measure of resource utilization, helping to standardize care levels across different patient scenarios․
5․3 Hybrid Approach to Level Assignment

The hybrid approach to level assignment in ED facility coding combines elements of both MDM-based and time-based methods, offering a balanced and comprehensive way to determine the appropriate level of care․ This approach recognizes that some patient encounters may not fit neatly into one category, as they may involve both complex decision-making and extended time spent in the ED․ By integrating these two aspects, the hybrid model ensures that the level of care reflects both the clinical complexity and the duration of services provided․ This method is particularly useful when one metric alone does not fully capture the patient’s needs or the resources utilized․ The hybrid approach enhances accuracy in coding and helps facilities reconcile cases where time and MDM do not align perfectly, ensuring proper reimbursement and reflecting the true extent of care delivered in the emergency setting․
